What's the difference between coronavirus ventilators, CPAP and BiPAP machines?
COVID-19 caused a shortage of ventilators so doctors are using other devices to treat patients
Get all the latest news on coronavirus and more delivered daily to your inbox. Sign up here.
As doctors face a shortage of ventilators that are crucial for treating coronavirus patients with respiratory problems, some hospitals are turning to other ventilation devices to do the same job.
This has sparked a new conversation about the difference between ventilators, Continuous positive airway pressure, or CPAP, machines and bi-level respiratory devices known popularly as bi-level positive airway pressure, BiPAP, machines.
American Association for Respiratory Care chief business officer Timothy R. Myers told FOX Business that the word BiPAP is a trade name from a ventilator company and gets misused all the time. This term should never be used in COVID-19 discussion unless speaking about Medtronic's mode on of ventilation, he said.
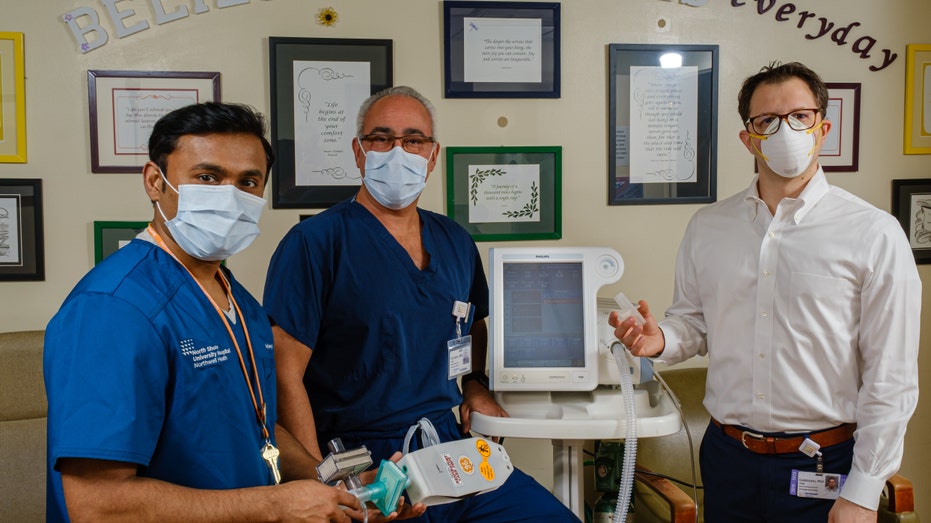
Drs. Stanley John, Hugh Cassiere and Todd Goldstein collaborated on turning BiPAP machines into backup ventilators. Photo: Northwell Health
Ventilators used in hospitals are bedside machines that help patients breathe when their bodies cannot do so on their own. The machines deliver oxygen to the body by invasive tubes that pass through a patient's mouth, vocal chords and into their lungs. Ventilators have various settings that can be adjusted based on a patient's condition, size and age.
CPAP and bi-level ventilator devices are typically used for sleep apnea, which is a sleep condition that causes one's breathing to stop and start irregularly. CPAP and bi-level machines are non-invasive, meaning they use a breathing mask to be put over a sleep apnea patient's nose to help with breathing.
CORONAVIRUS INSPIRES NY HOSPITAL SYSTEM TO MAKE BACKUP VENTILATORS FROM SLEEP APNEA MACHINES
CPAP machines only provide continuous flow and positive end expiratory pressures, or PEEP, AARC told FOX Business in a statement. The machines cannot be used for invasive ventilation on an intubated patient.
"Most cannot provide blended oxygen concentrations and have no ability to provide machine breaths to breathe for the patient. They also do not have monitor interfaces and most do not have alarms," the association explained.

Nurses in protective suits treat a patient in the intensive care unit at Ditan Hospital in Beijing, one of the hospitals in China's capital that are receiving COVID-19 patients.(Zhang Yuwei/Xinhua via AP)
Bi-level machines are different because, unlike CPAP machines that only provide a continuous flow of air and PEEP, these devices have two pressures including inspiratory and expiratory positive airway pressure, or IPAP and EPAP, AARC explained.
Because these devices have additional capabilities, AARC explained, many models are FDA approved for invasive ventilation and the others can be adapted under current federal regulations.
GM ADDS SECOND FACTORY FOR CORONAVIRUS VENTILATOR PRODUCTION
"Many hospitals have these in stock, but have traditionally never used them for invasive ventilation on intubated patients," the association added.
Yoel Hareven, the international director at Sheba Medical Center in Israel, which is at the epicenter of the COVID-19 pandemic in Israel, told FOX Business that Sheba is actively and successfully converting bi-level devices into ventilators for the hospital's patients.

Service Manager Keith Wilson tests a TV100 ventilator as President/ CEO Dean Bennett gives a tour of medical equipment manufacturer Bio-Med Devices to Governor Ned Lamont in Guilford, Conn. on Sunday, March 29, 2020. (Brian A. Pounds/Hearst Connectic
"BiPAP and CPAP machines absolutely can be useful in the fight against COVID-19," he said. "In recent weeks Sheba has converted these into life-saving devices in the fight against coronavirus and they are presently in use in our coronavirus unit."
All it takes to transform a bi-level device into a ventilator is some "relatively simple technical adjustments," Hareven explained. "In times of mass casualties, such as the current pandemic or times of war, BiPAP and CPAP machines can be rapidly converted into ventilators when there are not enough machines readily available."
TWITTER ATTACKS ELON MUSK FOR VENTILATION DEVICE DONATIONS
Yet, some medical professionals have their doubts. They say non-invasive CPAP and bi-level machines have the potential to spread COVID-19 if they are not converted properly into ventilators.
A March 27 NPR article that says non-invasive, bi-level and CPAP machines "could spread COVID-19" by aerosolizing the virus. The article gives the example of a nursing home in Washington state in which residents connected to CPAP machines contracted the aerosolized virus.

Staff work in a ventilator refurbishing assembly line at Bloom Energy in Sunnyvale, Calif. (Beth LaBerge/KQED via AP, Pool, File)
Dr. Mary Dale Peterson, the president of the American Society of Anesthesiologists, told FOX Business that certain CPAP and bi-level machines can be converted into ventilators with the right technology and procedures, but she has two concerns.
First, she explained the difference between CPAP and bi-level machines, saying CPAP machines only have one setting whereas bi-level machines have two so it can help inflate lungs.
GET FOX BUSINESS ON THE GO BY CLICKING HERE
The first concern with non-invasive, bi-level and CPAP machines is aerosolizing the virus and contaminating the atmosphere, as the NPR article notes. Additionally, "there is an expiratory gap on the machine where exhaled air goes, which is also a potential source of infection," Peterson said.
The second concern is that "a lot of COVID-19 patients that need this type of ventilation support" are probably better off using "the invasive part of ventilation and put a breathing tube in early on," she explained.
"Having said that, some of these machines can be really useful because they can be converted into a ventilator device," Peterson concluded.




















