Covid-19 Vaccines Are Getting Stuck at the Last Step
Local governments, hospitals and clinics have the doses, but not the resources to organize getting them to the right people
In South Texas, a man slept in his car for two nights straight so he wouldn’t lose his place in a line of hundreds of people at a mass-vaccination event. In Western Kentucky, residents registered for vaccination slots online, only to find when they arrived that their doses had been taken by walk-ins. In New Mexico, state officials scrambled to hire more people to staff a vaccination hotline after it was overwhelmed with callers.
The biggest challenges in America’s Covid-19 vaccination effort have turned out to be getting shots into the arms of the right people. As of Friday morning, some 31 million vaccine doses had been distributed nationwide, but only about 12 million had been administered, according to the Centers for Disease Control and Prevention.
The federal government shipped those doses to states around the country, with states establishing their own criteria for who should get the vaccine first. But it has been up to local health departments, hospitals and other providers to actually manage the tangle of logistics and many have been unable to do so effectively.
The result is an erratic and disjointed process that is causing frustration and confusion around the country.
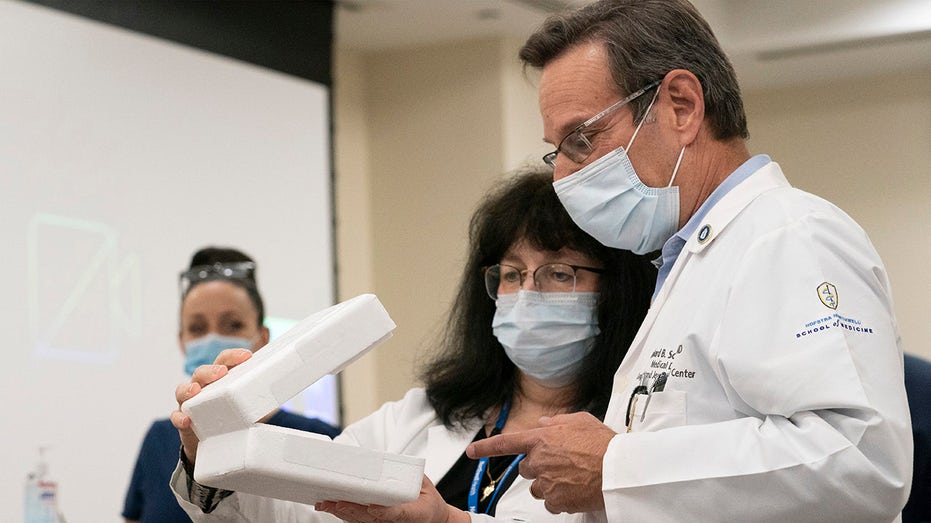
Pharmacy director Dana Rucco, center, shows medical director Richard Schwarz the container used to deliver the Pfizer-BioNTech COVID-19 vaccine, Monday, Dec. 14, 2020, at the Jewish Medical Center, in the Queens borough of New York. (AP Photo/Mark Le
Jeff Duchin, public health officer for Seattle and King County, Wash., said the federal government succeeded in helping fund and purchase vaccines that were developed in record-breaking time, but said it didn’t do nearly enough to ensure that the “last-mile” distribution efforts would be successful.
“Operation Warp Speed gave us two Cadillac vaccines with empty gas tanks,” he said.
Dr. Duchin said that while the county set up four clinics, it has been difficult to link health-care workers unaffiliated with hospitals to providers giving shots. Officials are currently planning two large-scale vaccination sites, he said, which are complicated to organize but are the most effective way to vaccinate teachers, transit workers, police and the general public. If everyone needs to schedule individual appointments, “we’ll never get there,” Dr. Duchin said.
Confusion is only increasing as many states move from immunizing health-care workers and nursing-home residents to people over 65 years old or with pre-existing conditions. California, Texas and Arizona are among states initiating mass vaccination sites in locations such as sports stadiums.
Providers across the country said they have thus far received little guidance for how to implement eligibility criteria, no funding to manage staffing and planning and no indication of how many doses they will receive at any time. Oscar Alleyne, chief program officer for the National Association of County and City Health Officials, said long lines and jammed phones show how responsibility was thrown on local officials without preparation.
MINNESOTA HOSPITAL FLAGS POTENTIALLY DEFECTIVE N95 RESPIRATOR MASKS: REPORT
“Most are struggling,” he said. “There is a lack of communication, a lack of understanding with the systems that have been developed, zero visibility into how the state plans are going to be implemented on the local front.”
Health officials said they hoped $8 billion in a recent stimulus package passed by the federal government would help local departments that have been underfunded for years. President-elect Joe Biden outlined a plan on Friday that includes federally supported community vaccination centers, mobile clinics to reach underserved populations, funding for more public-health workers and reimbursing states for deploying the National Guard to distribute doses.
Health officials with the Barren River District Health Department in Bowling Green, Ky., were looking at new software systems for scheduling appointments in mid-December when they found out doses were coming, forcing a quick choice, said Janarae Conway, disaster preparedness director. “We really did not have time to test it,” she said.
Administrators allowed the system to keep accepting online appointments after they had printed out a schedule, resulting in people showing up to see their slots were given away to walk-ins.
New Mexico secretary of health-designate Tracie Collins said her department was hiring more personnel after people recently couldn’t get through on phone lines when the state expanded eligibility to those over age 75.
MARK CUBAN LAUNCHES LOW-COST GENERIC DRUG COMPANY
Texas state Rep. Vikki Goodwin said that after the state granted eligibility to anyone over 65 on Dec. 28, her constituents rushed to call grocery stores and pharmacies for appointments only to be told there weren’t enough doses for that yet.
“It’s crazy that people have to call around to see what different providers have the vaccine, rather than having a central place,” Ms. Goodwin said. “People are thinking that we had months and months to prepare for this.”
Meanwhile, due to issues with Texas’s provider-approval system, some rural hospitals haven’t gotten vaccines for front-line health-care workers, according to the Texas Organization of Rural & Community Hospitals.
In South Texas’s Rio Grande Valley, Rolando Zarate, a 54-year-old diabetic, stocked his pickup with blankets and food before rushing to beat others to a mass-vaccination event. He received a shot after waiting 30 hours.
CHINESE CORONAVIRUS TESTS PUSHED BY US AGENCIES DESPITE SECURITY WARNINGS
“I have been, like most of the country, worried about [Covid-19] for nine months,” Mr. Zarate said. “I said, I don’t care how long I have to wait.”
The disorganization has resulted in some people who aren’t eligible getting vaccines through luck. When Seyward Darby saw a healthy, early-30s friend in Washington, D.C., post on Instagram that he had received one, she asked how. He said he had been picking up Hot Pockets to eat in Safeway when the store announced it had extra doses it needed to use, she said.
With limited guidance from states beyond the rules on who is eligible and limited resources for outreach, vaccine providers are in some cases not reaching everyone in the surrounding community, prompting concerns about health equity.
Ruben Becerra, the elected executive of Hays County, south of Austin, said some providers are focused on their own patients, excluding people without primary-care doctors.
“Some facilities have said ‘Well, you need to have a relationship with us and we need to do an assessment before we give you the vaccine,’” he said.
CLICK HERE TO GET THE FOX NEWS APP
In Washington, D.C., Dana Mueller, director of adult and family medicine at Mary’s Center, said the district has been submitting lists of people who signed up to get vaccines to the health center 24 hours in advance—not enough time for staff to set up an automated reminder call system. That has led to confusion over when people are supposed to show up and whether they have confirmed slots, Dr. Mueller said.
“It’s still very localized,” Dr. Mueller said. “It’s the small-scale effort that makes it feel like you’re going to be vaccinating people for years.”




















