UnitedHealthcare, Envision split: ‘Surprise’ medical bills on the way?
In ongoing negotiations over prices, UnitedHealthcare is warning patients it may drop Envision – the largest provider of emergency room doctors – from its coverage, in what could be a blow to patients.
United sent a letter to more than 350 hospital systems that it will terminate its contract with Envision at the end of the year unless new terms are reached: More than 950 hospitals would be impacted, the company said.
“Envision takes advantage of people when they are at their most vulnerable, in the emergency room, by price gouging patients,” a spokesperson for UnitedHealth said in a statement. “Envision is already charging more than two times the average cost of other ER physicians in UnitedHealthcare’s network and their greedy contract demands will hurt hospitals and consumers by driving up the cost of healthcare for everyone.”
If the talks fall through, more than 1 million UnitedHealthcare patients could be affected – and higher prices are likely to result.
“If UnitedHealth and Envision don’t reach an agreement, Envision says it will start whacking UnitedHealth’s subscribers with surprise medical bills,” Michael Cannon, a senior fellow at the Cato Institute, told FOX Business on Tuesday. “That’s a sleazy tactic when the prices Envision charges are far higher than the cost of providing those services.”
The price-gouging practice, not unique to Envision, is a result of the government-structured system, Cannon noted.
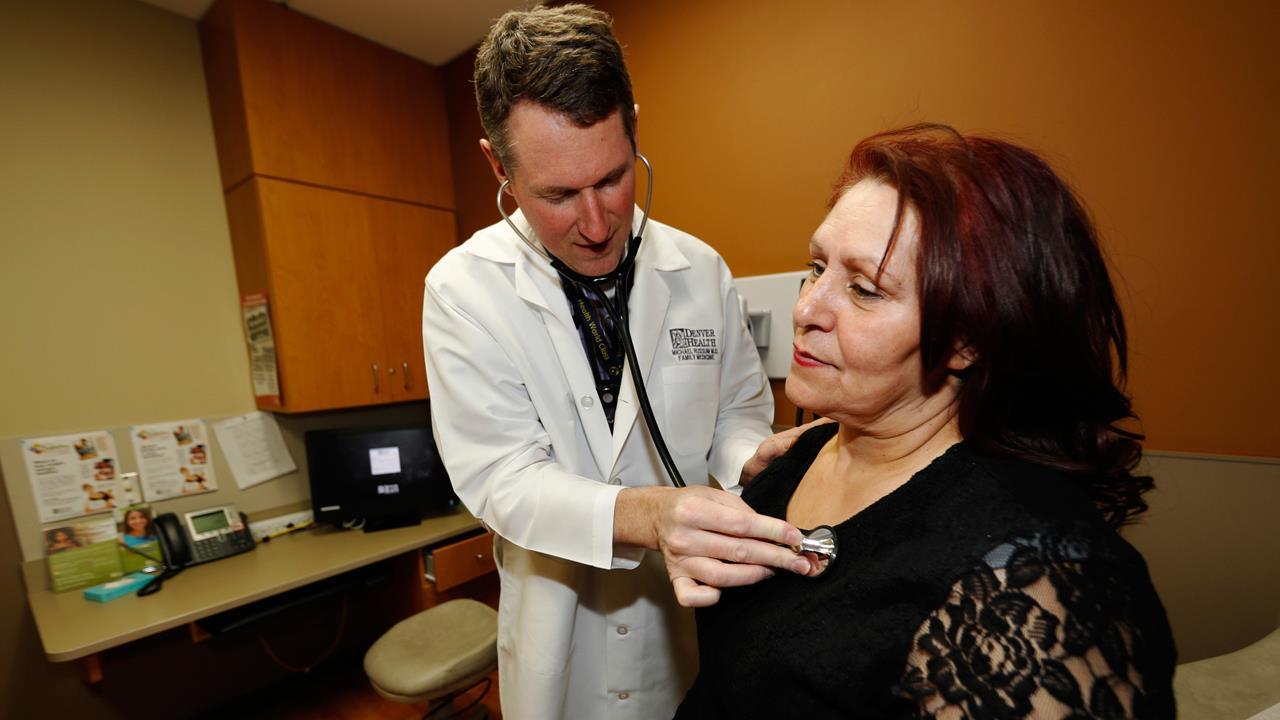
Many emergency room patients, as many as 20 percent, are treated by an out-of-network physician even if the hospital they go to is in-network, according to UnitedHealthcare. That’s because physicians independently contract with insurers and not the hospitals.
However, when patients visit the ER, they don’t have a choice of doctors.
Hospitals can charge inflated prices for out-of-network coverage, which can result in those costs being passed on to consumers.
“Congress penalizes workers unless they enroll in the health plan their employer chose. So workers can’t avoid Envision’s surprise medical bills just by switching to another insurance company, like they could in a free market,” Cannon said.
Envision maintains it has been negotiating “in good faith” with United, saying the insurer wants to “undo” progress between the two.
“There were never any problems until now, when United demanded massive cuts to allow us to stay in-network. We have offered United a solution that helps with the affordability of healthcare, and yet United is making egregious demands that will force all of our physicians out of network,” a spokesperson for Envision said in a statement.
The first hint of discord came last year, when UnitedHealthcare said Envision was overcharging. United says the provider charges “significantly higher rates for the same services,” which it claims are on average 975 percent of what Medicare pays for the same services.
United and Envision are expected to continue negotiating through year’s end.