Arkansas drops 4,300 from Medicaid plan over new work rules
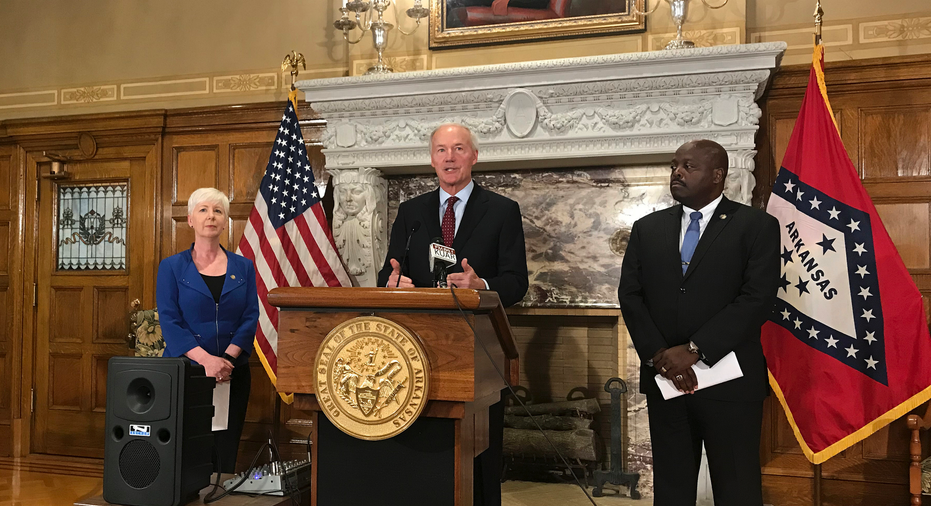
Arkansas Gov. Asa Hutchinson, center, talks at a news conference at the State Capitol in Little Rock, Ark., Wednesday, September 12, 2018, about the state's work requirement for its expanded Medicaid program. Officials said more than 4,300 people on the program lost coverage for not meeting the new work requirement. (AP Photo/Andrew DeMillo)
LITTLE ROCK, Ark. – Arkansas officials said Wednesday they've removed more than 4,300 people from the state's expanded Medicaid program who didn't meet a work requirement, making them the first in the nation to be kicked off Medicaid under a rule mandating they work to keep coverage.
The Arkansas Department of Human Services also said another 5,000 people on the program will lose coverage if they don't meet the work requirement by the end of this month. Of the more than 62,000 people who were subject to the requirement last month, officials said the majority either met the requirement or were otherwise exempt.
Republican Gov. Asa Hutchinson said he'd prefer to see more people complying with the requirement but defended the state's efforts to reach out to beneficiaries about the rule. Hutchinson has advocated for the requirements as a way to move people into the workforce.
"Compassion and common sense says that this is a good program for those who are trying to move up the economic ladder and better themselves," Hutchinson said. "It is also about providing assistance to those that need it and it is also about the value of work and responsibility."
Arkansas was the first state to implement a Medicaid work requirement after the Trump administration said it would allow states to require participants to work to keep coverage. Kentucky was the first state to win approval for a work requirement, but a federal judge blocked the state from enforcing it. A similar challenge over Arkansas' requirement is pending before the same judge.
Under Arkansas' requirement, beneficiaries must report at least 80 hours of work each month for three months in a year. The requirement only applies to the state's Medicaid expansion, which uses federal and state funds to purchase private insurance for low-income residents, and not the traditional Medicaid program. More than 265,000 people are on the state's Medicaid expansion.
"To me, Arkansas is definitely a cautionary tale for all of these work requirements and particularly in states that have features that are going to make it even more likely that large numbers are going to lose coverage," said Judy Solomon of the nonprofit Center on Budget and Policy Priorities.
Once fully implemented, Arkansas' requirement will affect able-bodied enrollees on the program, aged 19 to 49 years old, with no children. The requirement is being enforced on participants ages 30 to 49 this year and will expand to include those 19 to 29 years old next year.
Democrats and low-income advocates have said the state's requirement that the hours worked be reported through a website penalizes people without access to the internet.
"It's either stunningly bad, poorly designed, or it's meant to kick people off," Jared Henderson, a Democrat challenging Hutchinson in the November election, told reporters earlier Wednesday.
Hutchinson and state officials defended the online approach, saying that beneficiaries can also call one of 200 "registered reporters" at insurance carriers or other groups that can log in and report for them. The Department of Human Services said beneficiaries can also use computers at its county offices around the state.
"We always want to provide other avenues, and we've done that in this case," Hutchinson said.
___
Follow Andrew DeMillo on Twitter at www.twitter.com/ademillo