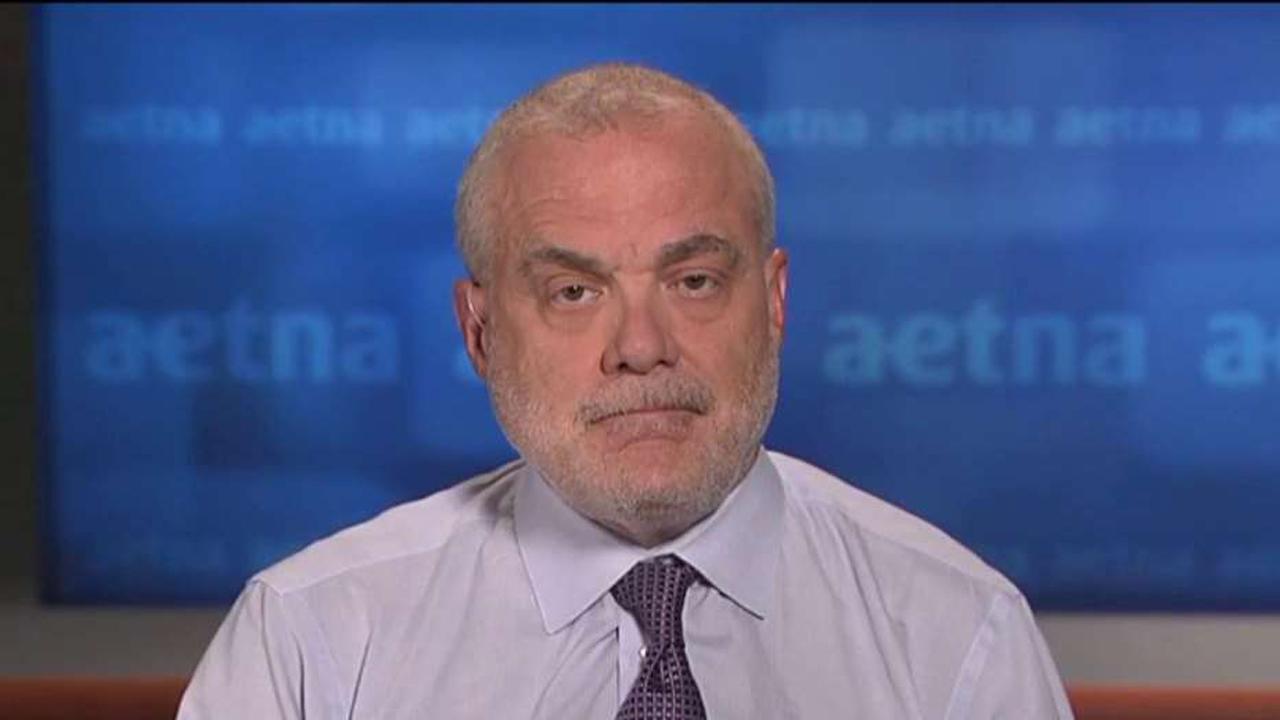
Aetna CEO: Expecting Merger with Humana By Year's End
Health care costs in the United States are plaguing both consumers and providers alike with the latest illustration of the trend coming from Aetna on Tuesday. In its second-quarter earnings filing, the insurance provider said it will pull out of planned 2017 expansion into Affordable Care Act exchanges.
The move came after announcements earlier this year from UnitedHealth (NYSE:UNH) and Humana (NYSE:HUM), which also announced plans to cut back on ACA exchange participation next year.
“While we are pleased with our overall results, in light of updated 2016 projections for our individual products and the significant structural challenges facing the public exchanges, we intend to withdraw all of our 2017 public exchange expansion plans, and are undertaking a complete evaluation of future participation in our current 15-state footprint,” Mark Bertolini, Aetna’s chairman and CEO, said in a statement.
Aetna, the nation’s third-largest health insurer behind UnitedHealth and Anthem (NYSE:ANTM), sells Obamacare plans in 15 states. Bertolini said the company has been hurt by the high cost of medications and procedures for customers in the exchanges.
“These people need these procedures and they need these drugs and they need to be covered,” he said. “But when you couple that with a risk-adjustment mechanism for high-risk people, that really is limited by virtue of the legislation, it causes everyone in the system to lose money.”
Bertolini said the exchanges could work if adjustments were made to the health-care law. In its current form, though, it’s nearly impossible.
“Modify [the legislation] to include risk adjustment that allows us to cover more sick people, which is what we want to do,” he said. “Which is what we do, by the way, in Medicare, and if we can get that structure proper then we’ll be just fine, we’ll be able to take care of everybody.”
On Tuesday, Aetna and Humana agreed to sell certain Medicare Advantage assets to Molina Healthcare. This comes after the two companies proposed a merger in late July. However, the Department of Justice filed a lawsuit last month in an attempt to stop Aetna’s takeover of Humana, saying the merger would create an anti-competitive environment. The DOJ filed a related suit to stop Anthem’s takeover of Cigna.
“When we’re both together, we’re 10% of the overall U.S. market and, at any given local market level no more than that, where the largest competitors are the Blues that have 50,60 and 70%,” Bertolini said. “So I don’t think we’re going to be all that omnipresent. I think we have a more national presence and an ability to provide product across the United States, which, for portable people, will be a really good thing.”
Bertolini outlined what the next president needs to do in order to make the exchange system more effective for all Americans who use it.
“Let’s take care of the people who are in the pool. Let’s recognize what their cost is. Let’s build the financing around it to do it. If we want to get younger people in the pool let’s create a separate set of products for them because they don’t need the kind of intensity that the current people do. Let’s admit who we’re covering, make the financing work and it will all come together.”
In the meantime, if other major U.S. health care providers decide to reevaluate their Obamacare exchange participation, more troubles may be on the horizon for customers. Jeff Loo, director of Healthcare Equity Research at S&P Investment Advisory Services said 2017 is adding up to be a “very challenging” year as large providers pull out of expanding their ACA offerings.
“You can have a lot of marketplaces without competition and it would raise costs due to a lack of competitors," Loo said. "It would put a lot of pressure on non-profits such as Blue Cross Blue Shield to participate in these markets. Some regional providers would need to step up as well.”