Penalty for refusing to get health insurance remains intact
WASHINGTON – Opponents of President Barack Obama's health care law who wanted to get rid of the penalty people were assessed for not having health insurance will have to wait longer for relief after the Senate early Friday defeated the GOP's scaled-back version of legislation repealing the Affordable Care Act. .
One of the main reasons GOP lawmakers had given in their quest to overturn "Obamacare" was that they want to lower premiums for people who buy individual health insurance policies, particularly constituents who get no help from the law's tax credits. Some states are facing a second year of double-digit hikes.
"There is no doubt whatsoever that premiums in the individual insurance market would go up," said Larry Levitt of the nonpartisan Kaiser Family Foundation. "There is irony here in that the mantra from Republicans throughout this debate has been the need to lower premiums, but this step would do just the opposite."
Premiums would have gone up because insurers feared that without the penalty and the health law's underlying requirement to carry insurance, some healthy people would drop their coverage. That would have left insurers with a pool of sicker, costlier customers.
How big an increase?
An analysis last year from the nonpartisan Congressional Budget Office estimated an increase of roughly 20 percent, and Senate Minority Leader Charles Schumer of New York says the budget office has told his staff that estimate still stands.
The CBO estimated this week that about 16 million people would become uninsured if the coverage requirement is repealed. Without the penalty, healthier people and those juggling tight household budgets might decide to take a chance and drop coverage.
The penalty for going without coverage last year was the greater of $695 or 2.5 percent of household income, due when taxpayers file their returns. The amount is adjusted annually for inflation, so it would be higher this year if the penalty stays on the books. According to the latest IRS figures available, about 6.5 million households paid the penalty for tax year 2015, averaging about $470 each.
Repeal of the penalty was the centerpiece of the GOP's so-called "skinny repeal" bill, the last-ditch effort to get legislation through the Senate that failed in the early morning vote Friday. The bill would have left most of the ACA intact, striking only some of its most unpopular provisions. Senate Republicans say it wasn't meant to be a final product, but, instead, a maneuver to advance legislation so a House-Senate conference committee can rework it into a comprehensive package. Indeed, some senators fear the House would suddenly pass the measure and declare victory.
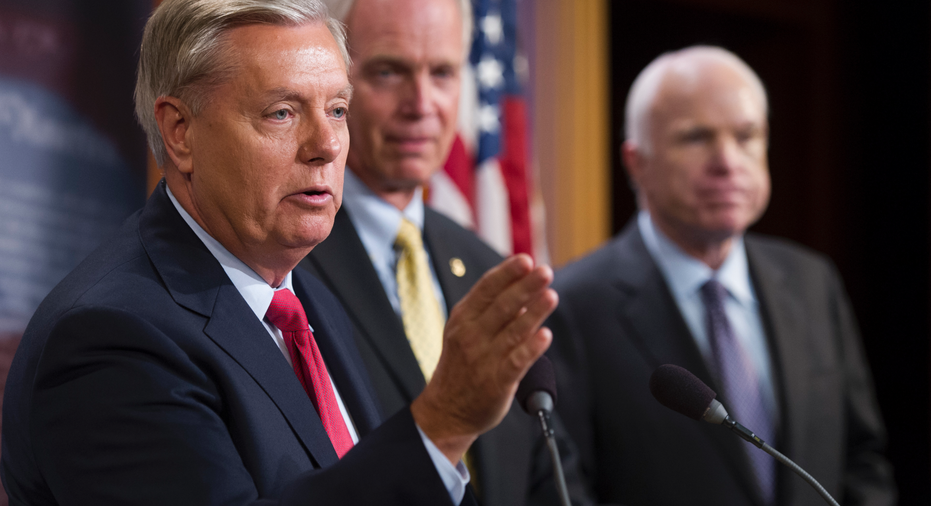
"I've told everybody this cannot be the final product," said Sen. Lindsey Graham, R-S.C.
"If you passed it as a stand-alone proposition it would destroy the insurance markets and we would own the failure of Obamacare," Graham added.
The health insurance industry opposed the provision.
Ten governors — five Republicans and five Democrats — have asked the Senate to drop the idea, warning it is "expected to accelerate health plans leaving the individual market, increase premiums, and result in fewer Americans having access to coverage." The governors want Congress to start over and try to come up with a bipartisan approach.
The unpopular penalty and coverage requirement were intended to nudge healthy people into the insurance market. They are modeled on an approach that Massachusetts passed in 2006 under former Republican Gov. Mitt Romney. The Massachusetts health overhaul had wide acceptance in that state, but the federal version under Democrat Barack Obama proved to be highly controversial.
Nonetheless, previous Republican health bills have recognized the importance of having some kind of penalty for people who don't maintain their coverage. Proposals have ranged from a surcharge on premiums to waiting periods. Something like that would likely be part of any final House-Senate legislation.
Those ideas are also unpopular with Americans. A recent AP-NORC poll found that 72 percent would oppose a six-month waiting period, and 67 percent would oppose a surcharge on people who had a break in coverage.
___
Associated Press writer Mary Clare Jalonick contributed to this report.



















