FDA approves coronavirus survivors' blood treatment in critical patients
The treatment, known as convalescent plasma, has been used before
Get all the latest news on coronavirus and more delivered daily to your inbox. Sign up here.
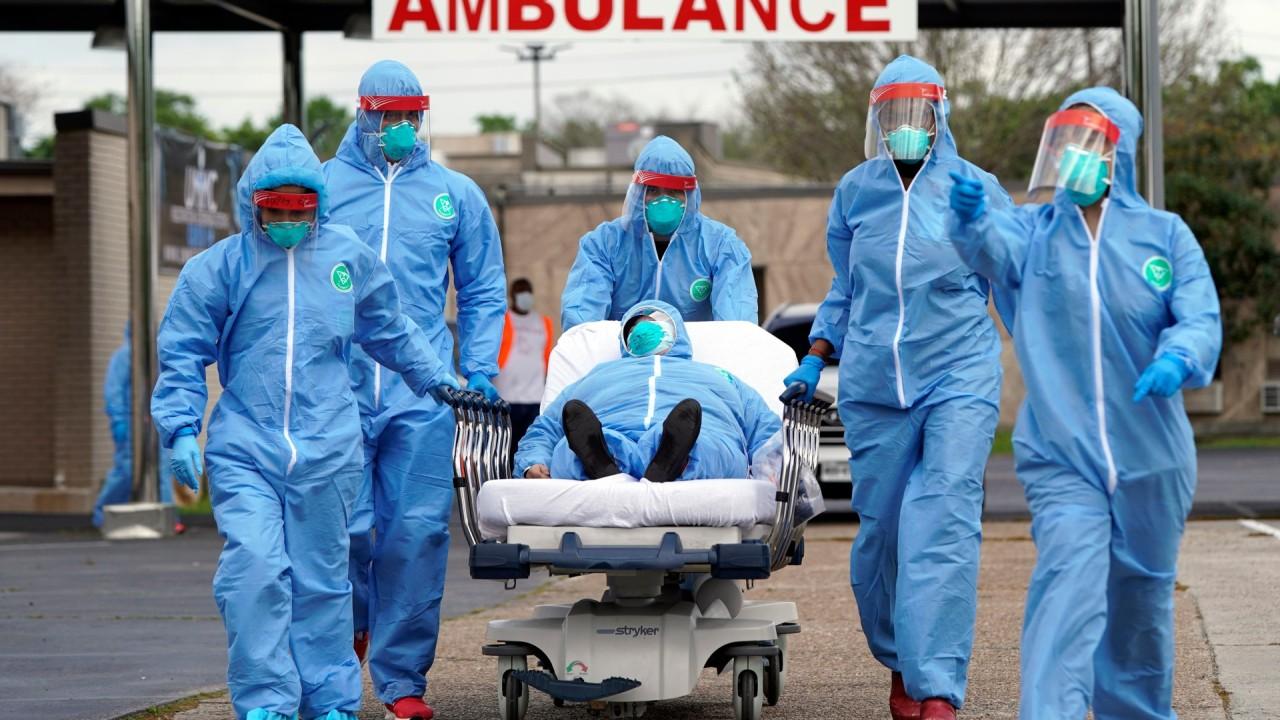
The Food and Drug Administration Tuesday approved new emergency protocols for the treatment of the coronavirus that will allow hospitals to use plasma donated by coronavirus survivors to treat critically ill patients with the disease.
It is a century-old treatment that has been used to fight off flu and measles outbreaks in the days before vaccines, and tried more recently against SARS and Ebola, just might work for COVID-19, too: using blood donated from patients who’ve recovered.
VIRTUAL VET VISITS ALLOWED DURING CORONAVIRUS, FDA SAYS
Doctors in China attempted the first COVID-19 treatments using what the history books call “convalescent serum” -- today, known as donated plasma -- from survivors of the new virus.
Still, there's no guarantee it will work.
“We won’t know until we do it, but the historical evidence is encouraging,” Dr. Arturo Casadevall of Johns Hopkins University’s school of public health told The Associated Press.
Casadevall drew on that history in filing the FDA application. The FDA is “working expeditiously to facilitate the development and availability of convalescent plasma" a spokesman said.
TRUMP TOUTS TELEHEALTH IN CORONAVIRUS PANDEMIC FIGHT
Here are some questions and answers about this latest quest for a treatment.
WHAT EXACTLY IS THIS POSSIBLE THERAPY?
It may sound like “back to the Stone Age,” but there’s good scientific reason to try using survivors' blood, said Dr. Jeffrey Henderson of Washington University School of Medicine in St. Louis, who coauthored the FDA application with Casadevall and another colleague at the Mayo Clinic.
When a person gets infected by a particular germ, the body starts making specially designed proteins called antibodies to fight the infection. After the person recovers, those antibodies float in survivors’ blood -- specifically plasma, the liquid part of blood — for months, even years.
One of the planned studies would test if giving infusions of survivors' antibody-rich plasma to newly ill COVID-19 patients would boost their own body’s attempts to fight off the virus. To see if it works, researchers would measure if the treatment gave patients a better chance of living or reduced the need for breathing machines.
One caution: While regular plasma transfusions are a mainstay of medicine, very rarely they can cause a lung-damaging side effect.
COULD IT ALSO ACT LIKE A VACCINE?
Sort of, but unlike a vaccine, any protection would only be temporary.
A vaccine trains people’s immune systems to make their own antibodies against a target germ. The plasma infusion approach would give people a temporary shot of someone else’s antibodies that are short-lived and require repeated doses.
Still, if FDA agrees, a second study would give antibody-rich plasma infusions to certain people at high risk from repeated exposures to COVID-19, such as hospital workers or first responders, said Dr. Liise-anne Pirofski of New York's Montefiore Health System and Albert Einstein College of Medicine. That also might include nursing homes when a resident becomes ill, in hopes of giving the other people in the home some protection, she said.
“We need both things desperately,” Pirofski said. “We need to be able to break the cycle of transmission and we also need to be able to help people who are ill.”
WHAT’S THE HISTORY?
These plasma infusions were used most famously during the 1918 flu pandemic, and against numerous other infections, such as measles and bacterial pneumonia, before vaccines and modern medicines came along. Long-ago research is sketchy. But in the Journal of Clinical Investigation earlier this month, Casadevall and Pirofski cited evidence that 1918 flu patients given the infusions were less likely to die. And a 1935 medical report detailed how doctors stopped a measles outbreak from sweeping through a boarding school using “serum” from prior patients.
The old-fashioned approach still is dusted off every so often to tackle surprise outbreaks such as SARS in 2002, and in 2014 when Ebola survivors’ plasma was used to treat other patients during the West Africa epidemic. Even during those recent outbreaks, strict studies of the technique were not done, but Casadevall said there were clues that the plasma helped.
UNITEDHEALTHCARE’S OXFORD UPDATES CORONAVIRUS INSURANCE POLICIES FOR EMPLOYERS
Casadevall thinks that when it didn't work, it may have been used too late. "Somebody at the end of their lives, it’s very hard to affect” any disease at that point, he cautioned.
A more modern approach is to brew this type of antibody in the lab, something Regeneron Pharmaceuticals and other companies are working on. Using blood from COVID-19 survivors is a decidedly more labor-intensive approach — but researchers could start banking the plasma as soon as regulators give the OK.
HOW WOULD DOCTORS GET THE PLASMA?
Blood banks take plasma donations much like they take donations of whole blood; regular plasma is used in hospitals and emergency rooms every day. If someone’s donating only plasma, their blood is drawn through a tube, the plasma is separated and the rest infused back into the donor’s body. Then that plasma is tested and purified to be sure it doesn't harbor any blood-borne viruses and is safe to use.
GET FOX BUSINESS ON THE GO BY CLICKING HERE
For COVID-19 research, the difference would be who does the donating -- people who have recovered from the coronavirus. Scientists would measure how many antibodies are in a unit of donated plasma — tests just now being developed that aren't available to the general public — as they figure out what's a good dose, and how often a survivor could donate.
Researchers aren’t worried about finding volunteer donors but caution it will take some time to build up a stock.
“I get multiple emails a day from people saying, ‘Can I help, can I give my plasma?’” Pirofski said.