Choosing Coverage in the Age of Health Care Reform
Confusion and cost concerns dominate the health insurance conversation for small-business owners. Here’s what you need to know.
The only thing certain since President Obama’s health care reform bill was passed 13 months ago is that nothing is certain.
“The reform has tossed health care into utter confusion,” says Bob Graboyes, senior health care advisor for the National Federation of Independent Business. “No one knows what the market is going to look like, so business is frozen.”
Choosing the right health care coverage for a small business right now is not only more confusing, but many experts say it’s also more costly for employers.
“Health care reform has increased the cost for employers across the board,” says Myron Jucha, vice president at Brooks Jucha & Associates, a San Diego-based employee benefits company. “We’re finding that insurance companies are raising the premiums dramatically because they don't know what the outcomes of the reform will be.”
With health care often the second-largest expense for a business after payroll, what’s a small business to do?
First we’ll give you a primer on what’s causing some of the confusion. Then we’ll tell you how to best manage the rising costs during this time of uncertainty.
Conquering the confusion
- Grandfathering regulations. Some say the new law states that you either need to stick with your old insurance plan without tweaking it, or step up to ones that’ll be more expensive, says Graboyes. Yet others say the grandfathering regulations don’t have much impact at all. Before you make any changes to your health plan, make sure you get a clear and concise answer to how these regulations may affect you.
- Exchange-driven process. The reform legislation requires that there be a health insurance exchange through which individuals and small businesses can purchase coverage. So far, however, the exchange process is one big question mark. “There are lots of other regulations that have to be written on what an exchange will look like, how it will be run,” says Graboyes.
Right now, it’s understood that the law requires people to either buy insurance or incur a penalty. Built into the law is an affordability standard that says if your income is below $88,200 per year for a family of four, you’re eligible for the exchange, explains Graboyes.
If you’re an employer and one of your employees requires this exchange, then you’re saddled with a penalty. “An employer has no way of knowing who’s entitled to a subsidy and who isn’t,” says Graboyes. Brokers are advising that you stay where you are and see where exchange regulations go.
Battling cost increases
- Assess your current plan. While most small businesses are in a holding pattern, it’s still a good idea to “make sure your plan meets your employee needs and promotes the enhancement that the reform has offered,” says Shawn Dangel, a small-business specialist with eHealthInsurance.
Most companies don’t know the extent of the benefits they offer. Even though a lot of companies want the stability of remaining with the same carrier, it’s important to take a good look at your plan and make sure it’s maintaining its competitive edge, and that the benefits are appropriate for your employees, says Dangel.
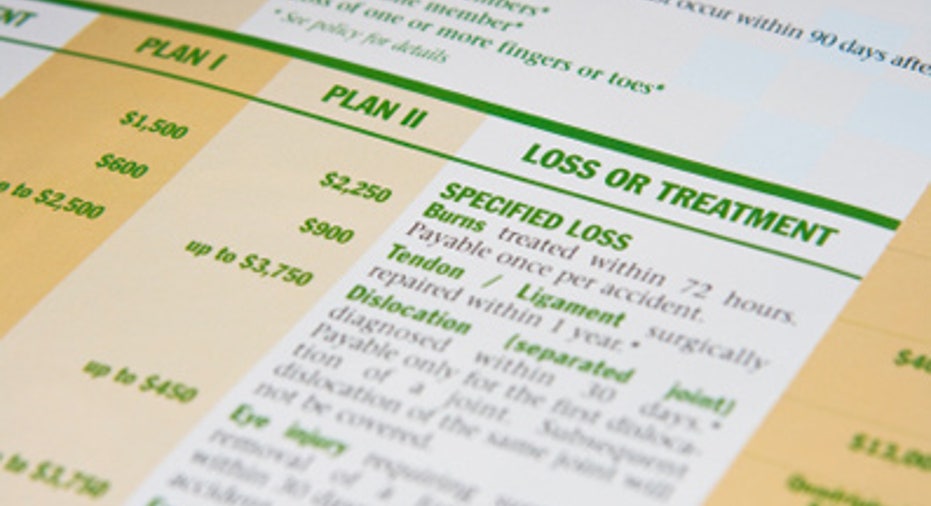
- Consider more modest benefits. Employees are aware that they need to share in the cost and be more selective in their health care choices. That is the whole idea behind the consumer-driven health care trend in which companies offer high-deductible health plans (HDHPs): low-premium/high-deductible plans in conjunction with health savings accounts (HSAs) or health reimbursement accounts (HRAs).
“Most employers are considering more modest benefits in the form of higher deductibles, or benefits that are HSA compatible,” says Dangel. “That’s the main way to offset cost increases.”
- Take on more risk. Many more small companies are moving to a self-funding model. In the past, companies didn’t want to take the risk — but now they’re saying that other options are too expensive. Prior to health care reform, “we would’ve never talked about this option with a company that had less than 250 employees, but now we’re talking about it with companies that have 30 employees,” says Jucha.
The self-funded model is based on the premise that a portion of the population will not use the plans as much as one might expect. “The 80 percent of the population that doesn’t use it will pay for the 20 percent that does use it,” says Jucha. With self-funding, the employer takes the first $5,000 to $30,000 of funds per employee per year and puts it into an account instead of giving the premium to an insurance company. At the end of the year, that account should have some money left over.
“One of our clients who moved to self-funding a portion of the deductible saved the company about 35 percent in premiums,” says Jucha. When he looked at this company a year later, of that 35 percent savings, the employer paid out 25 percent in claims and saved 10 percent overall.
To recap, Jucha recommends raising the deductible as high as comfortably possible, decreasing the premium, but then asking the employer to pay for it. The employer is taking on the risk from $250 to $10,000, which is less expensive and something that employers have been very willing to do.
Ultimately, with sound planning and open communication between employers and employees, it is possible to battle the confusion and cost increases.



















